Medical Networks
A medical network is a group of doctors, hospitals, and other providers that have agreed to accept a specific price for their services. PEHP has three networks – Summit, Advantage, and Preferred. A provider who is contracted in your network is an “in-network” provider. Get the best benefit by visiting doctors, hospitals, and other providers contracted in your network. Otherwise, you could be on the hook for unnecessary large bills. Find providers in your network in the PEHP Provider Directory.
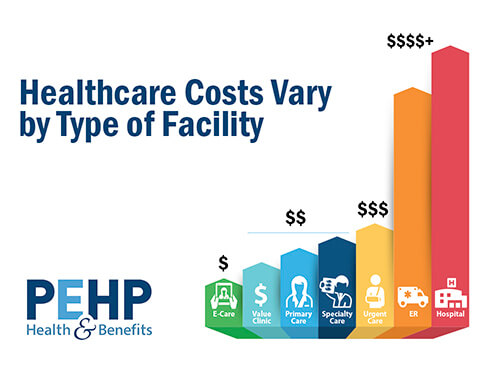 Where you get healthcare matters. Rates are always higher for medical services done at a hospital. Some services can only be done at a hospital but others, such as lab work, radiology, elective surgeries, and urgent care can be done in other settings.
Where you get healthcare matters. Rates are always higher for medical services done at a hospital. Some services can only be done at a hospital but others, such as lab work, radiology, elective surgeries, and urgent care can be done in other settings.
For lab work, let your doctor know you want to use an in-network lab that will forward the results to your doctor.
For radiology and certain elective surgeries, consider seeing in-network providers for substantial savings. For example, you could save $1,442 for an MRI at a large multi-specialty clinic.
Large multi-specialty clinics
- Revere Health
- Granger Clinic
- Tanner Clinic
- Ogden Clinic
If you don’t have a medical emergency but need immediate medical attention, visit the nearest Urgent Care Clinic. Also, consider consulting a doctor online with telemedicine.
PEHP divides providers into three categories for payment purposes: In-Network providers, Out-of-Network providers, and Non-Covered providers. Understanding the difference between the three categories will help you avoid billing surprises.
- In-Network Providers Paid at Contracted Rates
PEHP contracts with providers for two reasons. First, to get you the best rates possible. Second, to protect you from a provider demanding more than our contracted rate (balance billing).
Contracted rates can and do vary significantly. Be sure to use the PEHP Cost Tools to see price differences between facilities and providers of the same type.
- Out-of-Network Providers Paid at Lower Benefits (20%)
You might see an out-of-network provider by mistake or by choice. If you have Out-of-Network Benefits:
- PEHP generally pays 20% less than it normally would to a contracted provider.
- We credit 100% of the cost of seeing an out-of-network provider to your deductible up to the normal contracted rate.
- When you reach your out-of-pocket maximum, we still pay 20% less (80% rather than 100%).
- You don’t have to worry about balance billing for emergency services from an out-of-network hospital in Utah because of contracts we have in place.
If there’s a provider you like but not contracted with PEHP, you can nominate a doctor to add them to your network. If they agree on rates and meet our credentialing requirements, we’ll contract with the provider.
- Non-Covered Providers Paid $0
There are certain non-contracted providers that PEHP won’t pay anything even if you have out-of-network benefits. It doesn’t mean that you can’t receive services from them. It just means that PEHP will not pay any part of the bill.
Non-covered providers are mainly chiropractors, acupuncturists, drug screening laboratories, and residential treatment centers. There are also individual providers on the List who may put you at risk for overbilling, perform services that may not be medically necessary, or perform services generally not covered by PEHP. See the Non-Covered Provider List.
Some PEHP plans pay benefits for out-of-network providers. However, PEHP doesn’t pay for any services from non-covered providers, even if you have an out-of-network benefit.
Check your Benefits Summary to see if your plan has out-of-network benefits.
If it does, keep in mind you’ll usually pay a greater portion of the cost (co-insurance) for out-of-network providers. You may also be subject to balance billing. Balance billing happens when a provider not contracted in your network bills more than the allowed amount. For example, if the provider’s charge is $100 and the allowed amount is $70, the provider may bill you for the remaining $30.
To be covered, all out-of-network services must meet the same standard as if they were in-network. This means you must get preauthorization for certain services. All services must be medically necessary to be covered.
If a provider is not in your network, you will not be able to take advantage of PEHP’s discounts with the provider, and you may not know exactly how much the provider will bill. To avoid paying the full billed charges, PEHP encourages you to negotiate with the provider prior to services being rendered so that you will know exactly how much you will pay and may even receive an additional discount.
If you reach an agreement for the price of services with a provider, you may want to memorialize that in writing. PEHP has provided a sample agreement below that you may want to modify to fit your needs in such a scenario. PEHP provides this sample agreement as is, without representation or warranty of any kind. PEHP provides this sample agreement as information only. This information does not create an attorney/client relationship and is not intended to convey or constitute any legal advice. For legal advice, please consult a lawyer.